|
B
Balanitis | Baldness (go to alopecia)
| Basal cell cancer | Beau's
lines | Becker's naevus |
Behcet's syndrome | Birthmarks
| Bites, insect bites
and stings | Blackheads (go to comedones)
| Blisters | Boils (go to furuncles)
| Bowen's disease | Brittle
nails | Broken capillaries/veins (go to telangiectasias)
| Bromhidrosis | Bruises
| Bullous pemphigoid (go to pemphigus
and bullous pemphigoid) | Burns
and scalds
BALANITIS
The term, balanitis
refers to an inflammation of the foreskin and/or head of the
penis.
Causes
- Allergy to antiseptic
creams, spermicides and condoms (see contact
dermatitis).
- Fixed
drug eruption
affecting the penis.
- Skin diseases such
as psoriasis and lichen
planus.
- Candidiasis.
- Sexually transmitted
diseases such as herpes genitalis (see herpes
simplex virus infections), chancroid, syphilis and nonspecific
urethritis (NSU).
Symptoms
- Red dots.
- Red scaly patches.
- Swelling, cracks and
ulcers.
- Occasionally, discharge
of pus.
Complications
- Recurrent balanitis
can lead to a tightening of the foreskin, requiring circumcision.
What you can do
- You should consult
a doctor.
- Wash frequently with
saline prepared by dissolving a teaspoonful of salt in a pint
of water.
What the doctor
may do
- Perform tests to determine
the cause and treat accordingly.
TOP
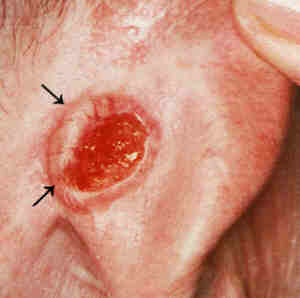
BASAL CELL CANCER
Basal cell cancers
(BCCs) or rodent ulcers are the most common type of skin cancer.
They usually occur on the sun-exposed areas of skin, especially
on the face, forehead, scalp and back of the hands. Fair-skinned
individuals, especially those of Celtic origin, albinos and those
heavily exposed to the sun are at higher risk of developing BCCs.
Causes
- Heavy occupational
or recreational exposure to the sun.
- Previous radiation
damage.
- Basal cell naevus
syndrome (rare inherited condition).
Symptoms
- A shiny bump that
is transluscent or pearly in appearance. Tiny blood vessels may
be seen growing over it.
- A small ulcer covered
by a crust and an elevated, rolled pearly border which may have
tiny blood vessels growing over it.
- Pigmented BCC shows any of the features
above but has brown or black pigment, as well.
- Morphoea-like BCC appears as a shiny whitish
scar-like area with blood vessels growing over it.
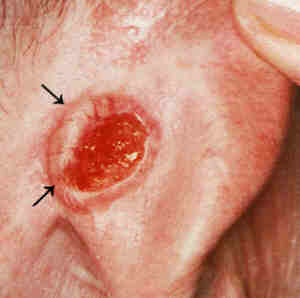 |
Basal cell cancer .
Click
on image for larger view. |
Complications
- Basal cell cancers
do not usually spread to distant sites but can spread deeper
or wider into the skin, damaging underlying tissues such as muscles
and bones and eroding into neighbouring structures such as the
eye.
What you can do
- You should consult
a doctor. Early basal cell cancers can be cured.
What the doctor
may do
- Perform a skin biopsy
to confirm the diagnosis.
- Excise with or without
skin grafts.
- Treat with , electrosurgery,
carbon dioxide laser,
liquid nitrogen, X-ray
therapy and Moh's chemosurgery.
- Counsel about sun-protection.
TOP
BEAU'S
LINES
Beau's lines are horizontal
depressions caused by a temporary disturbance of nail growth
as a result of acute illness such as measles, mumps, inflammatory
bowel disease, systemic lupus erythematosus
and heart attack or acute stress. It usually affects all the
nails. You should consualt a doctor to determine the cause. Treatment
is not necessary because the lines outgrow themselves.
TOP
BECKER'S
NAEVUS
This is a harmless
pigmented "birthmark" that appears around puberty.
It is more common in boys and usually occurs on the upper half
of the trunk, especially around one shoulder.
Cause
- A late onset pigmented
"birthmark".
Symptoms
- Light brown hairy
patch of irregular outline about the size of a hand or greater.
- The hairs may become
coarse with time.
What you can do
- You can consult a
doctor to confim the diagnosis.
- You can choose to
have treatment if it bother you.
What the doctor
may do
- Treat with carbon
dioxide laser.
TOP
BEHCET'S SYNDROME
This is a rare disorder
that involves the skin and other systems such as the joints,
eyes, mucous membranes of the mouth and genitalia, blood vessels
and the central nervous system.
Cause
- May be a autoimmune
disease (self allergy).
Symptoms
- Skin
- Vasculitis and painful
punched-out vasculitic ulcers (see vasculitis).
- Pustules (pusheads),
especially at venesection sites (where blood has been taken)..
- Erythema
nodosum (painful
nodules on the lower limbs).
-
- Superficial thrombophlebitis
(painful red nodules along the leg veins).
- Aneurysms (weakening
and dilatation of the arteries).
- Genital and mouth
ulcers.
- Arthritis (joint inflammation).
- Inflammatory bowel
disease with ulceration.
- Eye inflammation.
- Central nervous system
problems including encephalitis (brain inflammation), paralysis
and nerve palsies and psychiatric symptoms.
Complications
- Eye inflammation resulting
in blindness.
- Central nervous system
involvement may resulting in fatalities.
What you can do
- You should consult
a doctor as Behcet's syndrome may affect vital organs and cause
death.
What a doctor may
do
- Look for other organ
system involvement and treat accordingly.
- Prescribe oral steroids, azathioprine
(an immunosuppressive drug), colchicine (used to treat gout),
levamisole, chlorambucil (an immunosuppressive
drug), cyclosporin (a immunosuppressive
drug used to prevent the rejection of transplanted organs)
and thalidomide (used to treat hypersensitivity reactions in
leprosy).
- Treat ulcers with
intralesional
steroids injections.
TOP
BIRTHMARKS
Birthmarks may be caused
by a malformation of the blood vessels (vascular birthmarks or
haemangiomas) or the pigment cells or melanocytes (pigmented
birthmarks).
TOP
BITES, INSECT BITES AND STINGS
Insect bites and stings
vary in severity from mild localised to severe systemic life-threatening
reactions.
You have been bitten
by the brown recluse spider or the black widow spider.
You have generalised
urticaria, signs of anaphylaxis
developing , fever chills, weakness or vomiting.
What the doctor
may do
- Prescribe topical
or in more severe cases, even systemic steroids.
- Prescribe antibiotics
for infection.
- Institute emergency
measures for severe toxic or allergic reactions plus hospitalisation.
- Give desensitising
injections for bee and wasp venom allergy.
Prevention
- The only successful
way to treat bites and stings is to prevent them occuring in
the first place:
- Use screens and nets
to keep out mosquitoes and and other flying insects.
- Remove garbage and
cover food in order not to attract insects, particularly bees
and wasps.
- Eliminate the breeding
grounds of mosquitoes.
- Use insect repellents
to deter bites. Examples include DEET (diethyltoluamide) and
DMP (dimethyl phthalate).
- Consult a pest control
company to eliminate fleas and bedbugs.
- Have your pets examined
regularly by a Vet.
- Have the Ministry
of the Environment remove any bee and wasp nests near home.
- Carry an emergency
kit if you have severe life-threatening allergic reactions to
insect bites or stings.
TOP
BLISTERS
Blisters are collections
of fluid under the skin. In medical terminology, blisters less
than 1cm are called vesicles and those above are termed bullae
(singular bulla).
Causes
- Friction and pressure
from ill-fitting shoes, handling heavy tools.
- Insect bites and stings.
- Severe sunburn.
- Second
degree burns and scald.
- Acute
eczema of any
cause.
- Infections - herpes
simplex virus infection, chickenpox,
herpes zoster (shingles),
impetigo, a bacterial skin infection
and ringworm (see tinea).
- Rare blistering skin
diseases such as bullous
pemphigoid, pemphigus, epidermolysis
bullosa, porphyria cutanea
tarda, dermatitis
herpetiformis,
Complications
- Secondary bacterial
infection.
What you can do
- Keep the area clean.
- Do not break the blister.
Instead, protect it with a soft dressing. If the blister is large
or uncomfortable, pierce it on two sides with a needle previously
sterilised by flaming over a match to release the fluid. Do not
remove the blister roof as it serves as a biological dressing.
- Consult a doctor if
the blister is large, infected or the cause is uncertain.
What the doctor
may do
- Drain large blisters
under sterile conditions.
- Treat the underlying
cause.
- Prescribe antibiotics
for bacterial infection.
TOP
BOWEN'S
DISEASE
This is a type of squamous cell cancer
that has not invaded into the skin. It is also known as in-situ
squamous cell cancer.
Cause
- Chronic sun-exposure
- Chronic ingestion
of arsenic (previously used in some traditional asthma remedies).
Symptoms
- Reddish, slightly
scaly patch with sharp borders. It may be misdiagnosed as eczema.
- Erythroplasia of
Queyrat which
appears as a red, velvety patch on the penis (usually in the
uncircumcised) or vulva is also a type of Bowen's disease.
Complications
- Development into squamous cell cancer.
Squamous cell cancers arising from Bowen's disease are more aggressive
and more likely to spread to lymph glands.
What you can do
- You should consult
a doctor as soon as possible because early treatment can result
in cure.
What the doctor
may do
- Surgically remove
the abnormal area, use liquid
nitrogen, carbon dioxide
laser or electrosurgery.
TOP
BRITTLE
NAILS
This is a common problem
in women and has many causes.
Causes
- Excessive contact
with water, alkalis, detergents, solvents and other chemicals.
- Trauma.
- Polishes and solvents
used in nail polish removers.
- Nail hardeners and
false nails.
- Fungal nail infections
(onychomycosis).
- Iron deficiency anaemia.
- Old age.
- Circulatory problems.
- Skin diseases affecting
the nails such as eczema,
psoriasis and lichen
planus.
- Unknown.
What you can do
- You should consult
a doctor.
- Wear cotton lined
rubber or vinyl gloves to protect the hands against water, detergents
and soaps, and household cleansers.
- Minimise the use of
nail polish removers. Touch up chipped polish instead.
- Moisturise the skin
around the nails regularly.
- Avoid the habit or
pushing the cuticles back.
- Keep the nails short
in order to reduce trauma.
Keypoint
- Nail hardeners that
are meant to strengthen nails may actually be harmful.
What the doctor
may do
- Exclude skin diseases
affecting the nail such as onychomycosis,
eczema, psoriasis
and lichen planus.
- Treat underlying conditions.
TOP
BROMHIDROSIS
Bromhidrosis is the
medical term for body odour.
Cause
- Bacterial decomposition
of sweat produced by the apocrine glands (the special sweat glands
found in the armpits, nipple and pubic area).
What you can do
- You can consult a
doctor for treatment.
- Wear loose clothing
and shave off the hair to facilitate sweat evaporation.
- Omit foods that contain
garlic, onion and asparagus which are excreted in sweat.
- Bathe or shower regularly.
- Change clothes frequently.
- Use antiperspirants
to reduce sweating.
- Use deodorant soaps.
These work by leaving traces of antibacterial chemicals such
as triclosan and benzathonium chloride on the skin in order to
inhibit the action of bacteria. Do not use ordinary soaps afterwards
as these will wash the antibacterial chemicals away.
- Use talc to absorb
the sweat.
- Avoid hot environments.
- Limit physical activity,
if possible.
-
- What the doctor
may do
- Counsel on the above
measures.
- Prescribe antibacterial
soaps.
TOP
BRUISES
A bruise is a blue-black
discoloration caused by bleeding under the skin.
Cause
- Trauma.
- Blood disorders.
- Fragile blood vessels.
- Septicaemia (blood
poisoning).
- Drugs that affect
clotting such as aspirin, warfarin (blood thinning drugs).
Symptoms
- Initially blue-black
then yellow.
What you can do
- You should consult
a doctor if brusing is spontaneous or occurs after minor trauma.
- Application of a cold
compress or ice pack
after injury will help to prevent a bad bruise from forming.
- Vitamin C 500mg twice
a day may help to build up collagen which strengthens the blood
vessel walls.
What the doctor
may do
- Determine the cause.
- Perform blood tests
to look for underlying blood abnormalities.
TOP
BURNS AND SCALDS
Burns and scalds occur
in different grades of severity depending on the cause and the
duration of contact.
TOP |