|
D
Darier's
disease | Dermatitis herpetiformis
| Dermatofibroma | Dermatomyositis
| Dermatosis papulosa nigra
| Dermographism | Discoid eczema
(go to nummular dermatitis)
| Drug eruptions | Dry skin (go
to xerosis) | Dysplastic
naevi | Dysplastic moles (go to dysplastic
naevi)
DARIER'S DISEASE
Darier's disease or
keratosis follicularis is a rare inherited disorder of keratinisation
(the way the skin cells accumulate keratin as they approach the
surface). It usually begins around puberty and gets worse during
adult life.
Cause
- Inherited as an autosomal
dominant trait which means only one parent need to be affected
and half the offsprings will inherit the defective gene and develop
the disorder.
Symptoms
- A rash comprised of
greasy brown papules (pimply bumps) on the scalp. ears, face,
neck and upper trunk.
- The affected areas
tend to be moist and often give out a foul smell.
- Usually itchy.
- The rash is made worse
by the sun.
- The palms and soles
may be thickened.
- The insides of the
mouth may also be affected by white patches.
- The nails may be fragile,
short and relatively wide, notched and ridged and red and white
linear streaks.
 |
Darier's disease.
Click
on image for larger view |
Complications
- Secondary bacterial
infection.
- Kaposi's varicelliform
eruption, a widespread viral infection caused by the herpes
simplex virus.
What you can do
- You should consult
a doctor.
- Avoid excessive sun-exposure
and use sunscreens.
- Wet compresses help
to relieve itching and reduce crusting and odour.
- Take oral antihistamines
to relieve itching.
What the doctor may do
- Perform a skin biopsy
to confirm the diagnosis.
- Treat the complications.
- Treat with oral retinoids such as acitretin.
TOP
DERMATITIS HERPETIFORMIS
This is a rare disorder
that is extremely itchy. It may affect any age group but is more
common in young adults.
Cause
- Autoimmune disorder
(self-allergy).
Symptoms
- Clusters of tiny red
papules (pimply bumps), blisters or small weals.
- Severe itching or
burning so much so that all that remains to be seen are only
broken skin.
- Usually occurs on
the upper back, elbows, knees, buttocks, scalp, face and hairline.
- May be associated
with gastric atrophy and gluten intolerance.
Complications
- Males have a higher
risk of intestinal lymphomas.
What you can do
- You should consult
a doctor.
What the doctor
may do
- Take a skin biopsy
for routine histology and immunofluorescence (examination under
a special immunofluorescence microscope).
- Perform a small bowel
biopsy to detect gluten intolerance.
- Treat with dapsone
or sulphapyridine.
- A gluten-free diet
may help both the skin and gastrointestinal tract.
TOP
DERMATOFIBROMA
Dermatofibromas or
histiocytomas are harmless fibrous swellings usually found on
the arms and legs, especially in women.
Cause
- Unknown, may be an
unusual response to minor skin injury such as insect bites or
minor skin trauma.
Symptoms
- Skin coloured or yellow-brown
pea-size papule (bump), often with a darker border.
- Feels firm or button-like
when gripped between the thumb and index finger.
- It shows the dimple
sign. This means is that it dimples when the skin surrounding
it is squeezed inwards with the thumb and index finger.
- Painless.
 |
Dermatofibroma.
Click
on image for larger view |
What you can
do
- You should consult
a doctor.
- Request removal if
it bothers you.
What the doctor
may do
- Confirm the diagnosis.
- Remove it surgically.
TOP
DERMATOMYOSITIS
This is an uncommon
disorder affecting the skin and muscles.
TOP
DERMATOSIS PAPULOSA NIGRA
This condition is more
common in the dark-skinned and is believed to be a form of seborrhoeic keratoses.
Cause
- Unknown.
- A familial or racial
tendency has been observed.
Symptoms
- Small black or brown
papules (bumps) most frequently on cheeks and aound the eyes
and temples.
 |
Dermatofibroma.
Click
on image for larger view |
What you can
do
- Nothing as they are
harmless.
- Consult a doctor for
removal if they are cosmetically disturbing.
What the doctor
may do
- Treat with liquid
nitrogen
- Destroy with the carbon dioxide laser.
TOP
DERMOGRAPHISM
Dermographism is a
type of urticaria that is induced by stroking the skin.
- Cause
- Histamine and other
chemicals are released when the skin is stroked, resulting in
linear weals.
Symptoms
- Itching is the first
symptom followed by scratching which causes the scratch lines
to swell or weal.
- Dermographism may
be triggered by heat, rough textured fabrics, rough toweling
and pressure on the skin.
- Dermographism may
occur with other types of urticaria.
- Dermographism may
continue for years.
 |
Dermographism.
Click
on image for larger view |
What you can do
- You should consult
a doctor.
- Take antihistamines
to reduce itching.
- Avoid rough fabrics,
rough toweling and heat.
What the doctor
may do
- Prescribe antihistamines.
- Perform blood tests.
TOP
DRUG
ERUPTIONS
Drug eruptions are
one of the most common manifestations of drug allergy. They can
mimic any skin condition and vary from mild rashes to severe
reactions such as anaphylaxis,
angioedema and Steven's
Johnson's Syndrome. Diagnosis and management by a doctor
is imperative.
Cause
- A person may develop
an allergy to any drug taken by mouth or injected, including
one that has been used before without problems. Drugs that more
commonly cause rashes include penicillin and penicillin drugs
such as ampicillin, amoxycillin, sulphur drugs, nonsteroidal
anti-inflammatory drugs (NSAIDs), allopurinol (used to treat
gout), phenytoin and carbemazepine (a drug used to prevent epilepsy),
antimalarials such as chloroquine and hydroxychloroquine and
gold (used for treating rheumatoid arthritis).
Symptoms
- Measles-like (morbilliform)
rashes.
- Urticaria.
- Erythema
multiforme
- target or bull's eye rashes, particularly noticeable on the
palms and soles.
- Steven's
Johnson's Syndrome
- a severe type of erythema multiforme involving the mucous membranes
lining the inside of the mouth, the eyes and genital area. Associated
with fever and malaise (feeling of illness).
- Toxic epidermal
necrolysis (TEN)
- severe reaction in which the skin looks like it has been scalded.
The skin comes off easily leaving large raw areas and the eyes,
mouth and genital skin are often ulcerated. Fever, chills and
malaise accompany the rash. Causes include sulphonamides, NSAIDs
(nonsteroidal anti-inflammatory drugs), phenytoin (an anti-epileptic
drug), allopurinol (used to treat gout) and penicillin. Death
may result fluid and electrolyte imbalance, secondary infection
and organ failure.
- Fixed
drug eruptions
- erythema multiforme-like rashes which occur in the same location
each time the causative drug is taken.
- A lichen
planus-like rash known as lichenoid drug eruption may be
caused by drugs such as chloroquine (antimalarial drug), gold
(sometimes used in the treatment of rheumatoid arthritis), captopril
(used in the treatment of high blood pressure), streptomycin
(an anti-tuberculosis drug), lithium (used in the treatment of
manic-depressive states) and by colour developers.
- Erythroderma and exfoliative
dermatitis.
- Blisters.
- Acneiform eruption
- see acne vulgaris.
- Erythema
nodosum - red,
painful swellings on the legs.
- Pigmentation
- Purpura.
- Vasculitis
- Photosensitivity.
- Alopecia - see telogen effluvium
- Generalised
pruritus..
 |
Fixed drug eruption.
Click
on image for larger view |
 |
Morbilliform type of drug
eruption.
Click
on image for larger view |
Complications
- Anaphylaxis and angioedema.
- Involvement of other
organs such as the lungs, liver and kidneys with potentially
serious consequences.
What you can do
- Be aware of the possibility
of drug eruptions when taking medicines. Stop the medicine and
consult a doctor immediately if you develop symptoms of an allergy.
- If you have a history
of drug allergy, apply for a medical alert card or tag (see prevention).
Caution
- Some drugs are essential
and suddenly stopping them can cause a worsening of the condition
being treated. It is important, therefore, to see a doctor immediately
after stopping the drug to see whether the skin condition is
drug related and whether alternative medicines are available.
Prevention
- Avoid the drugs you
are allergic to.
- Apply for a medical
alert card and carry it on your person all the time. The application
form needs to be completed by your doctor, as well.
- Inform your doctor,
dentist and pharmacist each time you see them.
- Inform your relatives
about your drug allergy, as well.
What the doctor
may do
- Determine the cause
through careful history taking, physical examination and laboratory
tests.
- Remove the drug causing
the allergy.
- Prescribe topical
or systemic steroids and strong antihistamines.
- Some drug eruptions
are mild and clear within two weeks of cessation and hospitalisation
is not necessary.
- Hospitalise patients
with severe reactions.
TOP
DRY HAIR
Dry hair is caused
by underactive sebaceous (oil) glands.
Cause
- Over-exposure to the
sun, sunlamps, hair driers or curling irons.
- Underactive thyroid
gland.
- Anaemia.
Symptoms
- Coarse, dry, lustreless,
sometimes brittle hair that may be difficult to comb and which
tends to "fly-away".
What you can do
- Hold the hair drier
at least 6 inches away and dry hair partially, leaving it to
dry hair naturally or better still, avoid using hair driers totally.
- Use mild shampoos
for dry, damaged hair.
- Use conditioners.
- Comb hair gently with
a wide toothed comb.
- Keep the hair short.
What the doctor
may do
- Exclude underlying
medical problems that require treatment.
TOP
DYSPLASTIC NAEVI
Dysplastic naevi are
atypical moles. They are atypical or different from common moles
in two main ways. Firstly they are very numerous, sometimes more
than 100 and secondly they look different and show the features
mentioned in the ABCD guide of the
American Academy of Dermatology (see below). The main significance
of dysplastic naevi lie in the belief that there is an increased
risk of malignant melanomas (cancerous moles) developing compared
to common moles.
Cause
- Unknown or sporadic
dysplastic naevi where there is no family history.
- inheritance as in
the familial dysplastic naevi or dysplastic naevus syndrome where
in addition to having dysplastic naevi, there is a family history
of melanoma in two or more close relatives. Here the lifetime
risk of developing melanoma is almost 100%. Familial dysplastic
naevi have an autosomal dominant mode of inheritance which means
that the offsprings of an affected parent has a 1 in 2 chance
of being affected.
Symptoms
- Large number of moles
(sometimes in the hundreds) usually on the back, chest, abdomen
and extremities.
- Moles show the characteristics
mentioned in the American Academy of Dermatology's ABCD
guide:-
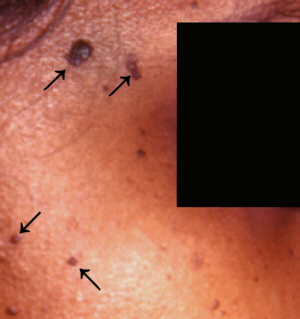
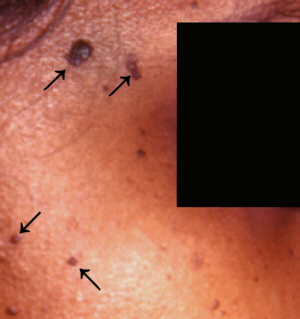
 |
Dysplastic naevi.
Click
on image for larger view |
Complications
- Development of melanoma.
The lifetime risk of developing melanoma has been estimated to
be 6% for sporadic dysplastic naevi and almost 100% for familial
dysplastic naevi.
What you can do
- You should consult
a doctor.
- You must take protect
your skin against sun-damage
- You should inform
your close relatives to go for a skin check-up as dysplastic
naevi may run in families.
What the doctor
may do
- Perform a careful
examination and biopsy (remove for examination) the more suspicious
moles.
- Follow up the patient
every 6 months to a year for life. It is often not possible to
remove all the moles because they are so numerous. Computerised
mole mapping systems are used in more specialised centres to
detect changes in moles.
TOP |