|
P
Papular
urticaria |
Parapsoriasis | Paronychia
| Pediculosis | Peels (see chemical
peels) | Pemphigoid (go to pemphigus
and bullous pemphigoid) | Pemphigus
and bullous pemphigoid | Perioral
dermatitis | Peutz Jeghers
syndrome | Photosensitivity
| Pigmentation (go to melasma)
| Pigmented purpuric
dermatosis | Pimples (go to acne
vulgaris) | Pitted keratolysis
| Pityriasis alba | Pityriasis
lichenoides | Pityriasis rosea
| Pityriasis rubra pilaris
| Pityriasis versicolor or tinea
versicolor | Poikiloderma
of Civatte | Polymorphic
light eruption | Pompholyx
| Porokeratosis | Porphyria
cutanea tarda | Portwine
stain | Pregnancy rashes
| Prickly heat (go to milaria)
| Prurigo nodularis
| Pruritus | Pruritus
ani | Pruritus vulvae
| Pseudofolliculitis
barbae (razor bumps) | Psoriasis
| Purpura
| Pyoderma gangrenosum
| Pyogenic granuloma
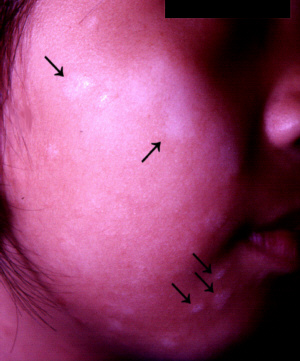
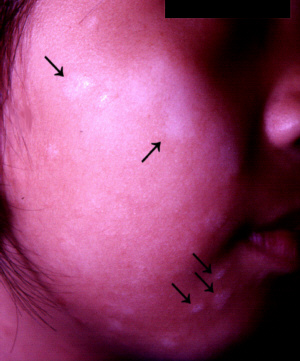
PAPULAR URTICARIA
Papular urticaria is
a condition that usually affects the legs and other exposed parts
such as the arms and face. It may affect any age group but is
more common in children.
Cause
- Insect bites eg.,
fleas and mites from infested cats, dogs and birds.
- Reaction to insects
or their products such as eggs and faeces.
Symptoms
- Crops of itchy papules
(bumps) and sometimes, blisters.
- Scratching leads to
crusting and open sores.
- New spots may reactivate
old ones.
Complications
- Infection due to scratching.
What you can do
- You should a doctor.
- Keep the house clean
and insect free.
- Keep pets outside.
- Keep pet houses clean
and pest free.
- Use insect repellents.
- Try to be as fully
clothed as possible.
- Take antihistamines
for itching.
What the doctor
may do
- Try to determine the
cause (which may not always be possible).
- Treat with topical
steroids or intralesional steroids.
- Treat infection with
antibiotics.
- Prescribe antihistamines
for itching.
TOP
PARAPSORIASIS
This consists of a
group of disorders that produce a persistent red scaly rash that
look a little like psoriasis (hence,
the name, "parapsoriasis". Some forms are harmless
but parapsoriasis en plaques is serious because it may progress
to mycosis fungoides,
a cutaneous (skin) lymphoma.
Symptoms
- Yellow-red to brown
slightly raised patches with a fine scale.
- Usually occurs on
the trunk, thighs and buttocks.
- May itch.
Complications
- Many develop into
mycosis fungoides.
What you can do
- You should consult
a doctor.
What the doctor
may do
- Perform a skin
biopsy to confirm the diagnosis.
- Treat with topical
steroids, UV-B
phototherapy or PUVA.
- Follow up closely
for development of mycosis fungoides.
TOP
PARONYCHIA
Paronychia is an inflammation
of the nailfolds. It may be acute or chronic.
Causes
- Acute paronychia is
caused by a bacteria, usually the staphylococcal or streptococcal
bacteria and occasionally, the pseudomonas and proteus bacteria.
- Chronic paronychia
may be caused by:
-
-
- Aggravating factors
- Frequent immersion
in water eg., in fishmongers, housewives, bartenders, and domestic
maids.
- Trauma such as pushing
and clipping the cuticles.
- Hangnails.
- Poor circulation.
Symptoms
- Acute paronychia -
severe throbbing pain, collection of pus or pus discharging from
under the nailfolds.
- Chronic paronychia
- red, tender swelling around the nails with discoloured, roughened
nails.
 |
Acute paronychia.
Click
on image for larger view |
What you can
do
- You should consult
a doctor.
- Paronychia cannot
be cured until a new cuticle forms to seal off the gap between
the nailfold and the nailplate. Careful nailcare and long-term
measures are necessary.
- Keep the hands clean
and dry. Avoid frequent handwashing and wear protective gloves
for wet chores (see hand
eczema).
- Keep the nailfolds
clean. Apply spirit lotion or some other antiseptic to prevent
acute infections.
What the doctor
may do
- Incise and drain the
collection of pus in acute paronychia.
- Prescribe oral antibiotics
for acute paronychia.
- Prescribe oral antifungals
in cases of candidal paronychia.
- Counsel about proper
hand care.
TOP
PEDICULOSIS
Pediculosis is the
medical term for louse infestation of the skin. The louse (singular
for lice) lives by biting and feeding on the blood it extracts
and can infest any part of the body that has hair. Three types
of lice infestation may be seen:
- Pediculosis capitis
(head lice) which affects the scalp and occasionally, the eyebrows
and eyelashes.
- Pediculosis corporis
(body lice) which affects the body.
- Pediculosis pubis
(pubic lice) which affects the pubic region primarily and the
lower abdomen, eyebrows, eyelashes and armpits occasionally.
-
- Causes
- Pediculosis capitis,
caused by the head louse can be transmitted by:
- Sharing combs, brushes
(especially by schoolgirls), hats and towels.
- Head-to-head contact.
-
- Pediculosis corporis,
caused by the body louse can be transmitted by:
- Sharing clothing or
other personal items.
-
- Pediculosis pubis,
caused by the pubic louse (crab louse) can be transmitted by:
- Sharing beds, clothing
or towels.
- Close physical contact,
eg., during sexual intercourse.
Symptoms
- Pediculosis capitis
-
- Itchy scalp.
- Presence of the lice
themselves.
- Nits (eggs) attached
to the hair. Although nits can resemble dandruff, they cannot
be flicked off or moved along the hair with the fingers. They
may sometimes be found on the eyebrows, eyelashes and beard,
as well.
- Groups of red itchy
papules (pimply bumps) on the neck.
-
- Pediculosis corporis
- Generalised itching.
- Red papules (pimply
bumps) and bloody crusts at the points where the clothes comes
into closest contact with the skin, eg., beneath collars, under
the belt, under underwear and in the armpits.
- Scratch marks, particularly
in between the shoulder blades.
- Pigmentation of the
skin may be seen in longstanding cases.
- Lice and nits are
usually found in the clothes, only rarely are they found on the
body hairs.
-
- Pediculosis pubis
- Affects the lower
abdomen, upper inner thighs and occasionally also the armpits,
eyebrows, eyelashes and hairline.
- Pubic itch.
- Red itchy papules
(pimply bumps).
- Scratch marks.
- Lice themselves.
- Dried specks of blood
on the underwear.
- Nits attached to the
pubic hair and occasionally, the eyebrows, eyelashes, armpit
hair and hairline of the scalp.
- Blue pigmentation
may be present over the lower part of the abdomen, upper inner
thigh and the armpits in chronic cases.
 |
Pediculosis pubis.
Click
on image for larger view |
Complications
- Secondary bacterial
infection.
What you can do
- You should consult
a doctor to confirm the diagnosis.
- Follow the doctor's
instructions on treatment. Do not overuse anti-lice medicines
as some of them are irritating to the skin and can be toxic.
- Take antihistamines
to relieve itching.
What the doctor
may do
- Look for nits or the
lice themselves. In pediculosis corporis, the nits and lice are
found in the seams of clothings rather than on the skin.
- Prescribe anti-lice
applications such as permethrin, benzyl benzoate, gamma benzene
hexachloride, pyrethrin with piperonyl butoxide and crotamiton.
- Prescribe antibiotics
for secondary infection.
Keypoints
- Family members require
treatment, as well. Sex partners of individuals with pediculosis
pubis (pubic lice) also need treatment. Classmates of those with
pediculosis capitis (head lice) need to be examined.
- In pediculosis corporis
(body lice), the nits and lice are found in the seams of clothings.
Clothing must washed in hot water or dry cleaned and the seams
must be ironed.
- Nits can remain on
the hair after successful treatment. These can be removed by
soaking the hair with 1:1 vinegar:water solution for 30 minutes
under a shower cap or towel and then combing through with a fine
toothed comb.
Prevention
- Avoid close contact
with infested persons.
- Avoid sharing hats,
combs, towels and other personal items.
- Bathe and change clothes
frequently.
- Avoid casual sex.
TOP
PEMPHIGUS AND BULLOUS PEMPHIGOID
These are skin diseases
that cause the skin to blister.
Cause
- Autoimmune (self-allergy)
disease in which antibodies are produced against the intercellular
cement which hold the epidermal cells together (pemphigus) or
the basement membrane which anchors the epidermis to the dermis
beneath (bullous pemphigoid).
- Inherited as in Hailey-Hailey
disease (familial benign chronic pemphigus).
Symptoms
- Pemphigus
-
- Multiple flaccid blisters
that rupture easily, leaving raw painful areas.
- Ulcers in the mouth.
- Usually affects the
middle-aged and elderly.
-
- There are several
types of pemphigus for example pemphigus foliaceus, pemphigus
vegetans, pemphigus vulgaris, pemphigus erythematosus and Hailey-Hailey
disease (familial benign chronic pemphigus).
-
- Bullous pemphigoid
-
- Itchy red patches
which later develop into tense, fluid-filled blisters.
- The blisters may also
develop on normal skin.
- The mouth is usually
not affected.
- Bullous pemphgoid
usually affects the elderly.
 |
Bullous pemphigoid.
Click
on image for larger view |
Complications
- More common with pemphigus.
- Secondary bacterial
infection which may lead to septicaemia (blood poisoning) and
fatality.
- Fluid and electrolyte
imbalance due to loss through the exposed raw skin.
What you can do
- You should consult
a doctor.
What the doctor
may do
- Admit for management.
- Prescribe oral steroids with or without
immunosuppressive
drugs.
- Prescribe antibiotics
for secondary infection.
TOP
PERIORAL DERMATITIS
This condition more
commonly affects in women in the 20s and 30s and may be mistaken
for acne vulgaris.
Causes
- The most common cause
is the inappropriate use of strong topical steroids on the face.
Other factors that may play a role include:
-
- Atopic tendency.
- Inadequate cleansing.
- Overuse of moisturisers,
foundation and sunscreens.
- Acne
rosacea.
- Candidiasis.
- Fluoride toothpastes.
- Sun-exposure.
-
- Symptoms
- Small red papules
(bumps) on a red scaly base.
- Occurs around the
mouth sparing a strip of skin near the lips.
- Occasionally, the
skin around the nose and eyes are also affected.
- Itching or occasionally,
a burning sensation can be felt.
 |
Perioral dermatitis.
Click
on image for larger view |
What you can
do
- You should consult
a doctor.
- Cleanse with mild
soaps.
What the doctor
may do
- Wean off or stop strong
topical steroids
(this is often followed by a temporary flare-up).
- Prescribe oral antibiotics
for 2 - 3 months.
TOP
PEUTZ JEGHERS SYNDROME
This is an inherited
disorder that causes freckles on the lips and gums and polyps
in the gastrointestinal tract.
Cause
- Inherited in an autosomal
dominant fashion which means the offspring has a 1 in 2 chance
of inheriting the disease from an affected parent.
Symptoms
- Appears in early childhood.
- Blue-brown or brown
freckles on the lips and mouth.
- Multiple polyps in
the gastrointestinal tract, especially in the small intestine
where they may cause abdominal pain, vomiting and haemorrhage.
Complications
- There is a 2% risk
of cancer developing in the polyp.
What you can do
- You should consult
a doctor.
What the doctor
may do
- Perform tests to exclude
intestinal polyps.
- Follow up closely
for the development of cancer.
- Us a pigment
laser to remove the freckles for cosmetic reasons.
TOP
PHOTOSENSITIVITY
Photosensitivity refers
to an abnormal sensitivity to sunlight. Sensitivity may occur
to ultraviolet B (short wave ultraviolet light that causes sunburn),
ultraviolet A (long wave ultraviolet light that causes tanning)
or even to visible light. Sometimes the sensitivity is so severe
that even artificial light sources such as fluorescent lamps
can cause it. Photocontact dermatitis is a type of
allergic contact dermatitis
which only occurs in the presence of light.
|
Drugs causing photosensitivity |
Action |
|
Amiodarone |
Heart medicine |
|
Chlorpropamide |
Antidiabetic medicine |
|
Frusemide, thiazides |
Diuretics (used to remove excess water from the
body) |
|
Griseofulvin |
Antifungal medicine |
|
Tetracycline, sulphonamides, nalidixic acid |
Antibiotics |
|
Phenothiazines |
Antihistamine, tranquilliser |
|
Psoralens |
Photosensitising medicine used in PUVA |
|
Tretinoin and isotretinoin |
Vitamin A acids (retinoids)
used in the treatment of acne |
TOP
PIGMENTED PURPURIC DERMATOSIS
This refers to a group
of disorders characterised by reddish-brown spots or patches.
They are caused by the leakage of blood through the tiny capillaries
the skin. Hence, it is also called capillaritis. The red
colour is due to the blood pigment, haemosiderin. Exactly why
the capillaries should become leaky is not known for certain
but a hypersensitivity reaction to viral infection, food additives
and medications have been cited. Types of pigmented purpuric
dermatosis include:
- Gougerot-Blum syndrome
(pigmented purpuric lichenoid dermatosis)
- Itchy red brown spots
and bumps that join together to form a thickened patch.
-
- Schamberg's disease
(progressive pigmented purpura)
- Flat red brown patches
with rust coloured spots that look like cayenne pepper on the
ouside.
- Not itchy.
-
- Majocchi's disease
(purpura annularis telangiectoides)
- Like Schamberg's disease
but with telangiectasias (dilated capillaries) and arranged in
rings.
-
- Itching Purpura
- Like Schamberg's but
is more widespread and itchy.
-
- Lichen aureus
- Patch has a yellowish
hue (hence the term aureus means golden).
- Usually occurs over
varicose veins.
Key point
- A similar rash has
been reported due to an allergy to some dyes used in khaki uniforms.
 |
Pigmented purpuric dermatosis.
Click
on image for larger view |
What you can do
- You should consult
a doctor.
- Wearing compression
stockings can help.
Treatment
- Reassure the patient
that it is mainly a cosmetic problem.
- Identify and remove
the cause, if any.
- Prescribe topical
steroids which
may occasionally help.
TOP
PITTED KERATOLYSIS
This is a relatively
common bacterial skin infection affecting the feet in people
with sweaty feet or who wear heavy shoes a lot. It usually affects
adolescents and young adults.
Causes
- Infection by a bacteria
such as Corynebacterium minutissimum and Dermophilus
congolensis.
- Infection is encouraged
by moisture and warmth so pitted keratolysis usually affects
the feet of people who wear heavy shoes and people with hyperhidrosis
(sweaty feet).
Symptoms
- Irregular white patches
with pits. The appearance is most dramatic when the feet is wet.
- Pitted keratolysis
usually affects the pressure areas of the feet such as the forefeet,
heels and toe pads.
- Hyperhidrosis (sweaty
feet) may be present.
- The feet may smell.
 |
Pitted keratolysis.
Click
on image for larger view |
What you can do
- You can consult a
doctor.
- Wear full leather
shoes (ie., leather uppers and soles) which allow the skin to
"breathe" or wear open footwear, whenever possible.
- Wear heavy shoes for
short periods at a time.
- Switch to cotton socks.
- Change socks frequently
and alternate between two pairs of shoes, allowing one to dry
completely before wearing.
- Replace old smelly
shoes.
- Wash with soap or
antiseptic cleanser twice a day.
- Use antiperspirants
to reduce sweating.
- Sprinkle dusting powder
or corn starch to absorb the sweat.
What the doctor
may do
- Prescribe oral antibiotics,
topical antibiotics or Castellani paint.
- Treat associated hyperhidrosis.
TOP
PITYRIASIS
ALBA
Pityriasis alba causes
pink slightly scaly patches which clear, leaving patches of paler
looking skin. The pink stage is mild and often go unnoticed.
Most patients are alerted by the pale patches. Pityriasis alba
usually affects young children and occasionally, young adults,
as well. It is more noticeable in darker skinned individuals,
especially after a spell in the sun. Pityriasis alba may affect
the face, neck, upper trunk and upper portions of the limbs.
Causes
- May be a mild form
of atopic dermatitis
or xerosis (skin dryness).
- The affected areas
are less able to tan compared to the surrounding skin.
Symptoms
- Pink, slightly scaly
patches initially. This stage often passes unnoticed.
- Pale patches appear
after the pink patches clear. This is the stage that most patients
notice and seek medical attention because of concerns about pityriasis versicolor, a fungal
infection that causes pale patches.
- The pale patches become
more obvious after exposure to the sun because the affected areas
tan poorly compared to the surrounding skin.
- Non-itchy.
- Pityriasis alba usually
clears after several months to years even without treatment.
 |
Pityriasis alba.
Click
on image for larger view |
What you can
do
- You should consult
a doctor to confirm the diagnosis.
- Use mild soaps.
- Apply moisturisers.
- Use sunscreens to
prevent the surrounding skin from darkening and accentuating
the pale patches.
What the doctor
may do
- Exclude other conditions
that cause pale patches such as leprosy,
pityriasis versicolor and
vitiligo.
- Prescribe mild topical
steroids.
TOP
PITYRIASIS LICHENOIDES
Pityriasis lichenoides
is an uncommon skin disorder that affects adolescents and young
adults. It occurs in two forms:-
- Pityriasis lichenoides
acuta et varioliformis (PLEVA) or Mucha Haberman disease.
- Pityriasis lichenoides
chronica (PLC).
Cause
- The cause is unknown
but it is generally believed to be a hypersensitivity reaction
to an as yet unidentified microorganism.
Symptoms
- Pityriasis lichenoides
acuta et varioliformis (PLEVA) or Mucha Haberman disease
-
- Crops of red papules
(bumps) which blister and crust over and heal, leaving depressed
scars rather like chickenpox.
- New crops appear as
old ones heal.
- PLEVA usually affects
the trunk and the insides of the forearms and back of the legs.
- The person usually
feels well, although occasionally, there may be a slight fever
or headache.
- PLEVA tends to be
very persistent.
-
- Pityriasis lichenoides
chronica (PLC)
-
- PLC causes small red
brown spots with an adherent scale that can be scraped off to
reveal a shiny brown surface. These scales are often referred
to as mica scales.
- PLC usually affects
the trunk and the insides of the thighs and forearms.
- The rashes take a
long time to clear, hence the name "chronica" and often
leaves a brown stain that may take months to fade.
 |
Pityriasis lichenoides.
Click
on image for larger view |
What you can do
- You should consult
a doctor.
- Moderate exposure
to the sun without getting burnt may help to clear pityriasis
lichenoides chronica.
What the doctor
may do
- Perform a skin
biopsy to confirm the diagnosis.
- The doctor may prescribe
topical steroids, antibiotics for 2 - 3 months or use phototherapy.
Pityriasis lichenoides is not, generally, very responsive to
treatment.
- If PLEVA is very persistent,
he may even prescribe methotrexate, an immunosuppressive
drug.
TOP
PITYRIASIS ROSEA
This is a relatively
common, self-limiting skin disorder that affects mainly children
and young adults.
Causes
- May be due an to infective
agent such as a virus.
- Secondary syphilis
and drugs such as barbiturates (a tranquilliser), metronidazole
(an antibiotic), gold (sometimes used for treating rheumatoid
arthritis), captopril (used for treating severe high blood pressure),
clonidine (used for treating high blood pressure) and penicillamine
(sometimes used for treating rheumatoid arthritis) have been
reported to cause a pityriasis rosea-like rash.
Symptoms
- Starts as a single
2 - 5 cm pink or brown patch with a fine scaly border on the
trunk, upper arms, neck and thigh. This patch is called the herald
patch because it is followed by a more generalised rash.
- The generalised rash
appears 5 - 10 days later on the trunk and upper portions of
the limbs. It is comprised of multiple pink, oval shaped patches
measuring 0.2 - 2 cm in diameter. The surface has a wrinkled
appearance and a fine "cigarette-paper" white scale
(known as a colarette) can be seen around the border. On the
trunk, the long axes of the rash run parallel to the ribs, resulting
in a "Christmas tree" pattern.
- Itching is usually
absent, although in a few individuals, it can be unusually severe.
 |
Pityriasis rosea.
Click
on image for larger view |
What you can do
- You should consult
a doctor.
- Although a viral cause
is suspected, isolation is not necessary.
- Mild exposure to sunlight
may help the problem clear faster.
- Take antihistamines
if itching is severe.
What the doctor
may do
- Exclude other causes.
- Prescribe topical
steroids.
- Use UV-B
phototherapy using to clear persistent cases.
TOP
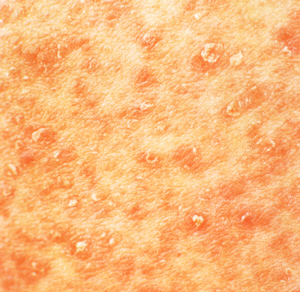
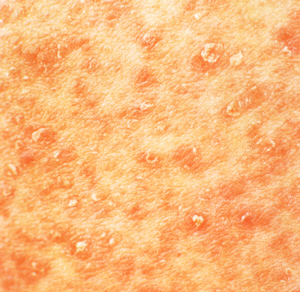
PITYRIASIS RUBRA PILARIS
This is a rare disorder
of keratinisation, the process by which cells accumulate keratin
as they reach the surface of the skin.
|