|
TREATMENTS
(Continuation of)
Finasteride | Hair
replacement surgery | Immunosuppressive
drugs | Implants | Intralesional
steroids | Lasers | Laser
resurfacing | Minoxidil | Phototherapy
| Retinoids | Sunscreens
| Previous ....
FINASTERIDE
Finasteride is a new
treatment for androgenetic
alopecia (male pattern baldness). It works by inhibiting
the 5-alpha reductase enzyme that converts testosterone to dihydrotestorone
(DHT). DHT is believed to suppress hair follicle activity so
that hair growth is retarded until eventually only a fluff of
hair is produced. Finasteride is taken orally at the dosage of
1mg per day. It takes about 6 months before any improvement can
be seen and treatment must be continued or the newly grown hairs
will fall out. Finasteride cannot be used in women that are or
may become pregnant because it may cause genital abnormalities
in male babies. In clinical trials comparing finasteride with
placebo (dummy pills), a small but slightly higher number of
men treated with finasteride noticed loss of libido (sexual drive),
erectile dysfunction and smaller volume of sperm. However, all
side effects resolved when finasteride was discontinued.
TOP
HAIR REPLACEMENT SURGERY
Medical treatments
of androgenetic alopecia
(male pattern baldness) with minoxidil applications or finasteride
tablets are effective only as long as the medication is continued
and hair will fall out once the medication is stopped. For those
who desire a more permanent solution and for those with severe
androgenetic alopecia, hair replacement surgery offers an alternative.
Hair replacement surgery may be divided into three main types
which may be combined to produce the best results.
- Hair transplantation.
- Flap surgery.
- Scalp reduction.
Hair transplantation
The hair at the back of the head are not affected by androgenetic
alopecia and can be relocated to the bald areas. This can be
done in two main ways - by removing grafts of hair-bearing skin
from the back of the head and inserting them in holes or slits
created in the bald area. The grafts differ in size and shape
according to the method used. Punch grafts are round and usually
contain 10 - 15 hairs, mini-grafts contain 2 - 4 hairs, micro-grafts
1 - 2 hairs, slit-grafts 4 - 10 hairs and strip grafts 30 - 40
hairs. The transplanted grafts retain the characteristics of
the hairs at the back of the head and are not affected by the
androgenetic alopecia. Hair transplantation is time consuming
and several sessions are necessary before the final result can
be seen. The new hairline is created and larger grafts are transplanted
during the initial session. The spaces between are filled in
by smaller grafts during subsequent sessions. The number of grafts
transplanted depends on the technique used, varying from 50 up
to 700 per session. Care is taken by the doctor to orientate
the grafted plugs so that the hairs will grow out in a natural
direction. The holes created in the back of the head are closed
by stitches. The scars are usually concealed by the hair.
Flap surgery
Flap surgery involves removing a flap of skin in the bald area
and creating a flap of hair-bearing skin that is slid across
and stitched into place, leaving one end still attached together
with its blood supply. Flap surgery allows large areas of hair
to be relocated but is technically more difficult.
Scalp reduction
This is a method to reduce the size of the bald patch rather
than replace hair. In scalp reduction, a section of the bald
scalp is removed and the surrounding skin is undermined (freed
from its deeper attachments) so that the edges can be brought
together and stitched. The procedure also gives the forehead
a slight lift. Doctors now combine different techniques and use
tissue expanders (a balloon-like device that is inflated with
saline to cause the skin to expand) to stretch the skin so that
larger sections of bald skin can be removed. Hair replacement
surgery is usually done under general anaesthesia or local anaesthesia
with IV sedation.
TOP
IMMUNOSUPPRESSIVE DRUGS
These are drugs used
to suppress the body's immune system. Immunosuppressive drugs
include corticosteroids which was described earlier and cyclosporin
(used to prevent organ rejection in transplant patients) and
some anti-cancer drugs. Immunosuppressive drugs are sometimes
used to treat skin disorders such as scleroderma, pemphigus,
bullous pemphigoid, lupus erythematosus, dermatomyositis, pyoderma
gangrenosum, Wegener's granulomatosis, some types of vasculitis,
mycosis fungoides, and even severe cases of atopic dermatitis,
psoriasis and alopecia areata. Examples of immunosuppressive
drugs include:
- Azathioprine.
- Hydroxyurea.
- Methotrexate.
- Cyclophosphamide.
- Cyclosporin (used
for treating organ rejection) is sometimes used to treat severe
atopic dermatitis, psoriasis, alopecia areata, ichthyosis vulgaris,
epidermolysis bullosa acquisita, pyoderma gangrenosum, systemic
lupus erythematosus, cutaneous T-cell lymphoma, sarcoidosis.Treatment
must be closely supervised and regular blood, urine tests and
blood pressure measurements are necessary. Side effects include
hypertension, kidney problems, increased hair growth, nausea
and loss of appetite, swollen bleeding gums and pins and needles.
TOP
IMPLANTS
Implants are synthetic
or natural materials that are implanted into the skin to improve
the facial contour or raise depressed or sunken scars and puff
up wrinkles. There are two varieties of implants - solid implants
and injectable implants:
- Solid implants
Solid implants are used to enhance the facial contour, for example
to strengthen the jawline or augment the cheek (known medically
as malar augmentation) or chin (mentoplasty) or reshape the nose
(rhinoplasty. Local anaesthesia with or without sedation or general
anaesthesia may be used. In chin augmentation for example, an
incision is made along the lower lip or under the chin and the
implant is inserted into a pocket created in front of the jaw
bone. For cheek implants, an incision is made inside the mouth
through the lower eyelid or behind the hairline. Recovery may
take 5 - 10 days, depending on the procedure. A variety of implants
may be used including bone, cartilage or silicone.
- Injectable implants
(filler techniques)
Injectable implants, as the name suggests are injected into the
skin to puff out wrinkles and raise depressed or sunken scars
with sloping edges (scars with well-defined steep edges do not
respond well). The material used for implants include collagen
purified from cattle skin, a material known as Fibrel, the patient's
own fat or a synthetic material known as Gortex but NEVER liquid
silicone.
-
- Collagen is injected into the dermis
and is available as Zyderm I and II and Zyplast. Zyderm collagen
is less concentrated and is injected into the upper layers of
the dermis. It can be used to correct superficial wrinkles on
the forehead, superficial or secondary creases adjacent to nasolabial
furrows, forehead creases, vertical creases around the lips which
cause lipstick to "bleed" and "crow's feet"
on the outside of the eyes. Zyplast collagen is more concentrated
and is injected into the mid to lower layers of the dermis. It
is used to correct deep wrinkles, nasolabial furrows which run
from the corners of the nose to the chin and deep distensible
scars (scars that are effaced when stretched) and for lip augmentation
(puffing the lips that are thinned and have lost their fullness
or pout). Zyplast cannot be used for treating deep forehead wrinkles
because there have been reports of it causing skin necrosis there.
How long the benefits of an implant lasts depends on the mobility
of the region. When used on a relatively immobile areas such
as acne scars, the benefits of an implant can last about 6 -
18 months. If the area is very mobile for example deep forehead
wrinkles and deep nasolabial furrows, the effect may last only
3 - 12 months. Crows feet can last up to 1 year. Lip augmentation
may only last 6 weeks. A skin test has to be performed by injecting
a small amount of collagen into the patient's forearm and checking
the site at 48 - 72 hours and then at 4 weeks. This helps to
detect allergy which occurs in about 3% of individuals. Very
occasionally, allergy may still develop in those whose skin tests
are negative. There is also concern that collagen might increase
the risk of autoimmune disorders (self-allergies) such as lupus
erythematosus, polymyositis/dermatomyositis developing. Collagen
implants cannot be used in pregnant women, people allergic to
lignocaine (the anaesthetic agent that is mixed in with the collagen
implant) or beef and in those with a history of autoimmune disorders
(self-allergies) such as lupus
erythematosus and rheumatoid arthritis.
-
- Fibrel contains three components
- a powdered gelatin made from porcine (pig) collagen, aminocaproic
acid and the patient's own plasma. Plasma is prepared from the
patient's own blood which means the doctor will have to draw
blood from the patient's arm. This is then centrifuged to separate
out the plasma which is then mixed with the gelatin and aminocaproic
acid. The mixture is then injected into the dermis. Fibrel is
useful for treating deep wrinkles and distensible scars, not
the more superficial facial lines. A skin test is still needed
to detect allergy even though this is less common than with collagen
implants. Fibrel injections tend to be more painful and the procedure
takes more time to perform and causes more bruising than collagen
implants. It is therefore, not as popular.
-
- Fat liposuctioned from the abdomen,
buttocks or thighs can be injected into the skin to replace fat
lost through ageing, puff up wrinkles and scars and to restore
fullness to thin lips. There is no risk of allergy since the
fat comes from the same person. The technique is known as autologous
fat transplantation. Fat cells are washed and decanted. 20 -
30% of cells will take, the others cells are absorbed. In a modification
of this procedure, called autologous collagen transplant, collagen
is extracted from the liposuction fat and this is then injected.
A US based company performs the extraction of collagen so this
technique is not available elsewhere. The benefits are similar
to those of cattle collagen except that there is no risk of allergy
since the collagen comes from the same person.
-
- Gortex is not truly an "injected"
implant but is included here for convenience. It is a synthetic
implant which has been used for many years in cardiovascular
and renal transplant surgery to serve as a channel between the
organ and the arterial supply and in surgery to repair hernias.
Recently, it has been used as a facial implant to augment or
plump up lips and to correct nasolabial furrows which run from
the corners of the nose to the chin and forehead furrows. In
nasolabial augmentation, for example, the strip of Gortex is
introduced with a needle and threaded underneath the skin. The
entry and exit points are then closed with absorbable sutures.
The implant does not dissolve and stimulates the production of
fibrous tissue which further augments the implant. The procedure
is usually done under local anaesthesia. It is generally safe.
Complications are uncommon and include infection, irritation
and rejection. Another similar but newer technique employs SoftForm
which comes as a round, spongy tube with a hollow core. It is
used in much the same way as Gortex and is quite good for softening
the laugh lines around the mouth and the from the corner of the
mouth to the chin.
TOP
INTRALESIONAL STEROIDS
These are injections
of steroids given directly into swellings such as keloids
and inflamed nodules and cysts due to acne vulgaris. The injection
is given through a very fine needle and causes a momentary stinging
sensation.
TOP
LASERS
- LASER is an acronym
for Light Amplification by
Stimulated Emission of Radiation.
Lasers use high intensity light of a specific wavelength to cut,
burn, coagulate (eg., blood vessels) or fragment (eg., melanin
or tattoo pigment).
The laser consists of an optical cavity or laser tube containing
the active medium (the source of the laser radiation) which may
be liquid (as in the flashlamp pumped dye laser), solid (as in
the Neodynium-Yttrium-Aluminium-Garnet or NdYag and Alexandrite
lasers) or gas (as in the carbon dioxide or CO2 laser), and a
power source to excite the atoms in the active medium. In accordance
with the laws of photophysics, excited atoms are unstable and
will return spontaneously to a more stable lower energy state.
When these atoms return to their steady state, they emit photons
of energy. Because there are thousands of atoms in the excited
state they tend to bump into one another transferring energy
to the other. Eventually some of the atoms reach energy levels
that exceed the threshold of a partially silvered mirror at one
end of the laser tube and are emitted as a high intensity laser
beam which can be used to destroy tissues and even cut metals
in industries.
There are many different types of lasers named after the active
medium used and the choice of laser depends on the type of tissue
being treated. Lasers may be classified into selective and non-selective
lasers:
-
- Selective lasers
In the skin there are various chromophores (light attracting
structures) such as oxygenated haemoglobin and pigment (eg.,
melanin or tattoo pigment) which absorb light of certain wavelengths.
It is possible therefore, to use lasers emitting light of a wavelength
that is absorbed by these chromophores to "smart bomb"
or selectively destroy these targets. These lasers are therefore,
termed selective lasers. Examples include:
-
- Vascular
lasers
-
- Flashlamp pumped dye
(585nm) laser
- Variable pulse width
NdYag (532nm) laser
-
- Pigment
lasers
-
- NdYag (532nm &
1064nm) laser
- Alexandrite (753nm)
laser
-
- Non-selective lasers
Sometimes the chromophore is present in all living cells like
water. Lasers that target water will therefore, destroy anything
in its path. Such lasers are termed non-selective lasers. Examples
include:
-
- Carbon dioxide
laser (10,600nm)
- Erbium Yag laser
The carbon dioxide
laser can
be used for cutting or burning skin growths. More recently, CO2
lasers have been introduced which are capable of producing a
very high energy output in short pulses of as little as 1 millisecond.
The high energy allows tissue to be destroyed in a shorter time
- milliseconds so that less heat is transferred to the surrounding
tissue, minimising the risk of scarring. These high energy pulsed
lasers are known as superpulsed or ultrapulsed lasers. The superpulsed
and ultrapulsed CO2 lasers have now been fitted with computerised
scanners which move the laser beam rapidly over the skin so that
the time the laser beam dwells on one particular spot is short
and even less heat is generated and consequently even less risk
of scarring. These lasers can remove layers of skin as little
as 50 - 100 microns at a time and can be used in more or less
the same way as chemical peels and dermabrasion to treat wrinkles
and scars (see laser resurfacing).
The Erbium-Yag laser removes even thinner layers of skin
(25 microns) and its main use is for laser resurfacing.
Selective lasers are
generally less painful and the application of an anaesthetic
cream 60 - 90 minutes beforehand will usually suffice. Non-selective
such as the carbon dioxide and Erbium-Yag lasers however, are
more painful and anaesthetic injections are usually required.
The different types of lasers and their uses are summarised below:
Lasers used
in Dermatology
|
Class of laser |
Examples |
Uses |
|
Vascular lasers |
Flashlamp pumped dye laser
(585nm)
Variable pulsed width NdYag laser
(532nm) |
Vascular birthmarks
Telangiectasias (broken capillaries)
Small varicose veins |
|
Pigment lasers |
NdYag laser (532nm) |
Red tattoos |
NdYag laser (1064nm)
Alexandrite laser (755nm) |
Pigmented birthmarks
Blue, black and green tattoos |
|
Non-selective
lasers
|
Carbon dioxide laser (10,600nm) |
Skin resurfacing.
Cutting and vapourising (burning) |
|
Erbium Yag laser |
Skin resurfacing. |
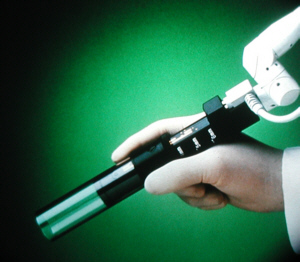 |
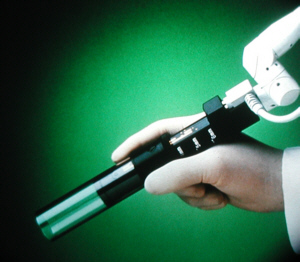
Laser used to treat pigmented
problems.
Click
on image for larger view |
TOP
LASER RESURFACING
The workings of lasers
were explained in the previous section. The carbon dioxide and
Erbium-Yag lasers can both be used to burn away thin layers of
skin. This technique, known as laser resurfacing or "laser
peeling" works like chemical peels
and dermabrasion.
The carbon dioxide laser is more deeply penetrating than the
erbium-yag laser which removes 25 micron layers of skin compared
to 50 - 100 microns by the carbon dioxide laser. Both these lasers
come with computerised scanners which scan the laser beam quickly
across the skin and allow the skin to be resurfaced quickly with
minimal heating of the skin and consequently, minimal risk of
scarring. Unlike dermabrasion, laser resurfacing is not hampered
by the spattering of blood and tissue and there is not much bleeding
to obscure the view. There is also less post-operative discomfort
and faster healing. Laser resurfacing is generally more expensive
than chemical peels or dermabrasion because of the high cost
of laser machines. The depth of penetration increases with the
number of passes the laser beam makes over the skin which allows
greater flexibility in treating different severity of scarring
and wrinkling. The benefits of laser resurfacing last an estimated
5 - 6 years. As with dermabrasion and chemical peels, deep ice-pick
acne scars require prior scar revision using punch excision,
punch elevation or punch grafting before laser resurfacing for
the best results. Remember also that the laser resurfacing only
pushes the age clock back, it doesn't stop it entirely. Treatment
may need to be repeated.
Benefits
- Improve wrinkles,
especially mild to moderate wrinkles and those around the eyes
(crow's feet) and mouth.
- Improve nasolabial
furrows and forehead frown lines.
- Improve scars caused
by chickenpox, surgery and trauma and some types of acne scars.
- Improve sun-damaged
skin.
Pre-treatment
This is similar to the preconditioning treatment described on
page . It has been observed that healing after laser resurfacing
is enhanced when the skin has been pre-treated with tretinoin
0.025 or 0.05% nightly so most doctors put their patients on
this regimen for 2 - 4 weeks prior to treatment. If hyperpigmentation
is anticipated, especially with skin phototypes
III and IV, the doctor may prescribe a lightening cream, as well.
Patients with a history of recurrent herpes
labialis (cold sores) and those having laser resurfacing
around the mouth are usually started on antiviral medicines such
as acyclovir or famcyclovir one day before surgery and continued
for a total of 7 - 10 days.
- Anaesthesia
Depending on the extent of the area being treated, general anaesthesia,
local anaesthesia or nerve blocks with or without IV sedation
may be used.
Laser procedure
- The face is cleansed
with a non-flammable cleanser to remove makeup, oil and dirt.
- You will then be asked
to wear protective goggles. If the area being treated is near
the eyes, special eyeshields need to be worn.
- The wrinkles may be
outlined prior to the local anaesthetic injections (because the
injections alter their appearance) and the area of treatment
delineated.
- The laser beam is
delivered to the skin via a special handpiece which is moved
over the treatment area with minimal overlapping.
- After each pass of
the skin, the doctor uses a saline-soaked gauze to wipe away
the burnt tissue. A dry gauze is then used to dry the area.
- Additional passes
are made to smoothen out wrinkles and scars, as necessary.
- The doctor may apply
a dressing over the area or he may use an open dressing method
involving the application of an antibiotic ointment or vaseline
several times a day.
It takes approximately
45 minutes to treat the areas around the eyes and mouth or 1
1/2 hour to treat the whole face. Laser resurfacing may be repeated
after 6 - 12 months, if necessary.
-
- Post-operative
course and care
Lasers produce a second degree burn and the wound must be properly
cared for in order to prevent complications.
- Swelling or oedema
may be severe especially around the eyes. You should be accompanied
by someone if you are not being hospitalised for the first few
days. Sleeping with the head slightly elevated for the first
3 - 5 days helps to reduce the swelling.
- Dry ice packs can
be applied (over the dressing, if any) as often as is necessary
during the first 3 days and paracetemol can be taken for pain
relief. Avoid taking aspirin or aspirin-like drugs.
- Dressings, if used,
are replaced after 24 hours and removed after 48 hours.
- The skin may be weepy
and crusts need to be removed because they form a medium for
bacterial growth. Crusts can be removed gently after soaking
the skin in cool or tepid water (some doctors advise adding some
vinegar) several times a day followed by application of the antibiotic
ointment of vaseline. Keep the skin moist at all times as it
speeds up the healing process.
- The newly resurfaced
skin is very red and this may last for 2 months or more. The
redness can be camouflaged with green foundation, followed by
a skin coloured make-up over it.
- Hydroquinone lightening creams can be resumed
after the skin has resurfaced and tretinoin cream 2 - 3 days
later.
- Avoid excessive exposure
to the sun and use sunscreens especially when the skin is still
red because pigmentation may develop. UV protective sunglasses
should also be worn after laser skin resurfacing around the eyes.
- Avoid strenuous physical
activity for at least 5 days and alcohol which may increase blood
flow and encourage the development of telangiectasias
(broken capillaries).
- The benefits of laser
resurfacing may not be apparent until some 2 - 4 months after
surgery so don't despair.
- Most patients can
return to work after the swelling has subsided in 7 - 10 days.
Complications
Although laser resurfacing is relatively safe, our skin's ability
to heal varies so the outcome is not always predictable. However,
serious complications are uncommon.
- Redness is expected
and is not really a complication of treatment. It lasts 6 -12
weeks after resurfacing. Green cosmetics are good for camouflaging
the redness.
- Scarring is uncommon
but may occur when the procedure is carried out too deeply or
if the wound gets infected. Early indications of the possible
development of keloids
(lumpy scars) include redness, elevation and itching of the skin
after it has apparently healed. Early treatment with steroid
creams may reduce the severity. The risk of scarring may be increased
in patients recently treated with isotretinoin which is why laser
resurfacing is normally performed at least 12 - 18 months after
completing isotretinoin treatment. Areas such as the upper lip
and jawline are more prone to develop scarring.
- Ectropion (pulling
away of the lower eyelid) may occur when laser resurfacing is
done too soon after blepharoplasty (eyelid surgery).
- Hypopigmentation (reduced
pigmentation) may occur with deep resurfacing.
- Hyperpigmentation
(increased pigmentation) may develop people with skin phototypes
III and IV. It is usually temporary and can be treated with lightening
creams as in melasma together with strict avoidance of sunlight
(see melasma). It may be avoided
with the use of preconditioning treatment.
- Bacterial infections
are rare and can be treated with antibiotics.
- Candidiasis a fungal infection caused
by a yeast-like fungus called Candida albicans is a rare
complication. It can be treated with antifungal medicines and
creams.
- Herpes labialis may recur after laser resurfacing which
is why patients with a history of herpes labialis are started
on anti-herpes medicines 1 day before resurfacing and continued
for a total of 7 - 10 days.
- Milia or tiny whitehead-like cysts
may occur transiently. They can be extracted with a number 11
scalpel blade. Pre-treatment of the skin with tretinoin helps
to reduce the formation of milia.
- Acne flares may occur
and can usually be treated with topical or oral antibiotics.
TOP
TOPICAL
MINOXIDIL
Minoxidil is a drug
used for the treatment of hypertension. One of its side effects
is increased hairgrowth which was why its manufacturer, Upjohn
formulated a topical form for the treatment of alopecia (hairloss).
It is used for the treatment of androgenetic
alopecia in both men and women and for alopecia areata. Topical
minoxidil is available in 2%, 3% and 5% strengths. To be effective
topical minoxidil must be applied twice a day for at least 4
months. Treatment must be continued or the regrown hairs will
slowly fall out again. Other than local irritation, topical minoxidil
does not cause any serious side effects.
TOP
PHOTOTHERAPY
Phototherapy uses light
for treatment. There are two main forms of phototherapy that
are used for treating skin disorders. Special phototherapy units
(cabinets) are used and 2 - 3 treatments per week may be necessary
for 12 - 24 weeks.
- UVB phototherapy
- using ultraviolet B light.
- PUVA (psoralen ultraviolet A) phototherapy
- using psoralens (chemicals that make the skin sensitive to
UVA) . in combination with ultraviolet A (UVA) light. It involves
applying the psoralen about 10 minutes before (topical PUVA)
or taking the psoralen 2 hours before shining.
UVB
phototherapy
- Uses
-
- Side effects
- Sunburns.
- Photoageing and increased
risk of skin cancers. Regular checkups for skin cancers are necessary.
- Eye damage such as
keratitis or an inflammation of the cornea and cataracts. Special
goggles are worn during treatment.
PUVA
- Uses
-
- Side effects
- Burns ranging from
a mild sunburn to blistering (topical and systemic PUVA).
- Tanned skin locally
(topical PUVA) or all over (systemic PUVA).
- Photoageing and increased
risk of skin cancers (systemic PUVA). Regular check up for skin
cancers are necessary for those undergoing phototherapy.
- Itching (systemic
PUVA).
- Nausea (systemic PUVA).
- Skin ageing
and increased risk of skin cancers (systemic PUVA). Regular checkups
for skin cancers are necessary.
- Eye problems such
as keratitis or an inflammation of the cornea and cataracts (systemic
PUVA). Special goggles are worn during treatment.
-
- Precautions to observe
whilst undergoing phototherapy (UVA or PUVA)
- Follow the doctors
instructions carefully.
- Phototherapy increases
the risk of photoageing (sun induced ageing) and skin cancers.
Protect the skin against natural sunlight and use sunscreens
religiously.
- Wear wrap around sunglasses
that protect against UVA and UVB.
- Inform your doctor
if you have sensitivity to the sun or are taking medications,
some of which may increase the sensitivity to sunlight.
- Tell your doctor if
you are pregnant. Systemic PUVA is generally not used in pregnant
women even though there is no evidence that PUVA affects pregnancy.
TOP
RETINOIDS
Retinoids refer to
drugs derived from vitamin A. There can be classified into topical
and oral retinoids.
Topical retinoids
- Tretinoin cream and
lotions - used for treating acne
vulgaris (pimples) or photoageing.
- Adapolene gel - used
for treating acne vulgaris.
Precautions to observe when using topical retinoids
- Use at night because
retinoids increase the sensitivity to sunburn. Use more frequently
only is instructed by your doctor. Adopolene does not seem to
increase the sensitivity to the sun.
- Apply to dry skin.
Wait at least 30 minutes after washing.
- Avoid the eyes and
mouth.
- Use sunscreens during
the day.
- Irritation may occur
and acne may get worse during the first 6 weeks of treatment
with tretinoin (less common with adapolene) but the skin usually
gets used to it. You may use moisturisers if the skin is very
dry but choose an oil-free or non-comedogenic one if you have
oily skin or acne vulgaris.
- Use mild cleansers
and avoid abrasive scrubs.
- Do not use during
pregnancy.
- Seek you doctor's
advice if you are uncertain about anything.
Oral retinoids
- Isotretinoin (Roaccutane
or Accutaine) - a very effective medication for nodular of cystic
acne vulgaris.
- Acitretin (Neo-Tigason)
- used for treating disorders of keratinisation such as psoriasis,
Darier's disease, pityriasis rubra pilaris,
etc.
TOP
SUNSCREENS
- Sunscreens, as the
name suggest filter or block the sun's ultraviolet light. They
can be divided into two groups:
- Physical sunscreens
(sunblocks) - Sunblocks block everything out and use opaque particles
such as zinc oxide and titanium oxide. These used to be messy
to use but many modern sunblocks now use micronised zinc and
titanium oxide which are do not leave such an obvious trace on
the skin.
- Chemical sunscreens
- These use chemicals that absorb light energy and dissipate
in an another form which is less harmful.
- Many modern sunscreens
contain sunscreen chemicals as well as sunblock agents to provide
broad spectrum protection. The ingredients commonly used
in sunscreens and sunblocks include the following:
UV-B screening chemicals
- PABA and its esters,
for example, glyceryl PABA, Padimate O and Padimate A
- Cinnamates such as
potassium cinnamate, diethanolamine-p-methoxy cinnamate, octyl-p-methoxy
cinnamate.
- Salicylates such as
octyl salicylate, omomenthyl salicylate, ethylhexyl salicylate
UV-A screening chemicals
- Benzophenones which
filter only short-wave UVA, for example oxybenzone, dioxybenzone
and sulisobenzone.
- Dibenzoyl methanes
which filters both short and longwave UVA, for example butylmethoxydibenzoylmethane
(Parsol 1789 or avobenzone), Parsol 8020 and Eusolex 8020.
- Meroxyl SX
Physical sunblocks
(blocks everything)
- Titanium dioxide
- Zinc oxide
- Iron oxide
TOP |