|
A
(continuation of)
Androgenetic
alopecia |
Angioedema | Angiokeratomas
| Angular cheilitis | Annular
erythema | Aphthous ulcers
| Aplasia cutis | Athlete's foot
(see tinea pedis) | Atopic
dermatitis | Atopic eczema (go to atopic
dermatitis) | Atrophie blanche
| Previous .....
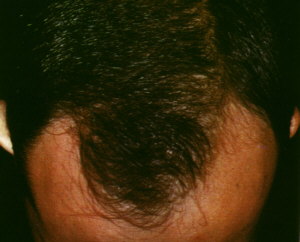
ANDROGENETIC ALOPECIA
This is a very common
type of hairloss known also as common baldness, male pattern
baldness and female pattern baldness. It may begin early as after
puberty.
Causes
- Androgens (male hormones).
- Inherited sensitivity
of the hair follicles to androgens.
- Symptoms
The symptoms may differ in men and women:
- Male androgenetic
alopecia (male pattern hairloss)
-
- Begins as a receding
hairline around the temples, producing an M-shaped pattern. Then
thinning or a bald patch develops at the crown. In severe cases,
these areas merge leaving a horseshoe rim of hair at the back
and sides of the head.
-
- Female androgenetic
alopecia (female pattern hairloss)
-
- May follow the pattern
in men or more commonly, as diffuse thinning which is most prominent
on the top front of the scalp.
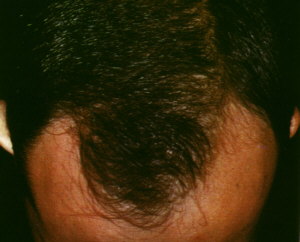 |
Male androgenetic alopecia.
Click
on image for larger view |
What you can
do
- Nothing, live with
it.
- Consider cosmetic
measures such as having a hairdresser style the hair so that
it hides the hairloss, hair weaving or using a hairpiece.
- Consult a doctor for
treatment.
Key points
- Women with androgenetic
alopecia who have the following symptoms should consult a doctor
for tests to exclude increased production of male hormones:
- Severe acne.
- Hirsutism.
- Enlargement of the
clitoris.
What the doctor
may do
- Confirm the diagnosis.
- Prescribe minoxidil
lotion or finasteride
tablets which may reduce the rate of hairloss or induce some
hairgrowth.
- Oestrogens (female
hormones) and antiandrogens tablets may be helpful in women.
- Consider surgery such
as scalp reduction
and hair transplantation in very motivated patients.
TOP
ANGULAR
CHEILITIS
Cheilitis refers to
inflammation of the lips. Angular cheilitis is a type of cheilitis
affecting the corners of the mouth.
Causes
- Chapping from cold
dry environments.
- Atopic cheilitis (exfoliative
cheilitis) which is a type of atopic dermatitis affecting the
lips (see atopic dermatitis).
- Drugs such as isotretinoin, a vitamin
A acid used to treat severe acne.
- Contact cheilitis
(a type of allergic or irritant contact
dermatitis affecting the lips) due to lipsticks, lipbalms,
toothpastes, foods, saliva (lip licking cheilitis).
- Cheilitis glandularis.
Symptoms
- Red, scaly, cracked
lips.
- Redness, swelling
and blistering may be seen in contact cheilitis.
- Cracks with scaling
at the corners of the mouth in angular cheilitis.
- Swollen lips with
numerous pinhead sized openings of the salivary glands in the
lips may be seen in cheilitis glandularis.
- Itching.
- Pain.
 |
Cheilitis
Click
on image for a larger view |
Complications
- Secondary bacterial
infection.
What you can do
- You should consult
a doctor.
- Avoid lip licking.
- Avoid eating acidic
foods or insert directly into the mouth without touching the
lips.
- Use vaseline to moisturise
the lips.
What the doctor
may do
- Determine the cause
and eliminate it.
- Diagnose and treat
complications.
- Perform patch or prick
tests to detect allergies.
- Prescribe a mild topical
steroids.
- Give intralesional
steroid injections in cheilitis glandularis.
TOP
ANGIOEDEMA
This is a type of urticaria involving the deeper parts
of the skin and mucous membranes. It may be life threatening
when it affects the throat as it may cause suffocation and death.
Causes
- Allergy, for example
to food products, drugs, insect bites.
- Inherited angioedema which is caused by the lack
of a C1 esterase inhibitor, an enzyme that keeps the complement
system in check. The complement system controls the production
of chemicals that cause inflammation.
Symptoms
- Large swellings in
the skin and and mucous membranes. On the face, it may cause
swelling of the eyelids and lips and severely distort the facial
contours. In the throat, the swelling may cause difficulty breathing
and suffocation.
- Abdominal cramps,
nausea and vomiting due swelling in the mucous membrane lining
of the intestines.
- Burning pain and occasionally,
itching.
Complications
- Impairment of vision
due to swollen eyelids.
- Breathing difficulties,
wheezing and suffocation when it affects the throat.
- Death from suffocation.
What you can do
- Go to the nearest
Accident and Emergency department.
What the doctor
may do
- Administer antihistamines,
adrenaline and corticosteroids
and insert a breathing tube or perform a tracheostomy (create
a hole in the windpipe) if there is suffocation.
- Determine the cause
so that future attacks can be avoided.
- Prescribe danazol
in cases of inherited angioedema.
TOP
ANGIOKERATOMAS
Angiokeratomas are
red-purple bumps. Most angiokeratomas occur for no known reasons
and are few and generally harmless. Some angiokeratomas are more
widespread and these may be associated with a genetic disorder
known as Fabry's disease.
Cause
- Unknown.
- Due to Fabry's
disease (angiokeratoma corporis diffusum) which is inherited
as an X-linked recessive disorder. X-linked means the defect
occurs in the X chromosome and only males are affected and women
are carriers.
Symptoms
- Red-purple raised
spots on the body, scrotum or hands and feet.
- Fabry's disease is
associated with heart and kidney disease and high blood pressure
and widespread angiokeratomas.
Complications
- Only occurs in Fabry's
disease because of heart and kidney involvement. Death may result
from kidney or heart failure.
What you can do
- You should consult
a doctor.
What the doctor
may do
- Exclude the Fabry's
disease which causes kidney and heart problems.
- Remove angiokeratomas
using lasers, electrosurgery
or surgical excision.
TOP
ANNULAR ERYTHEMA
Annular means ring-like and erythema
means reddish. Annular erythema, therefore is the term used for
a group of skin disorders characterised by reddish ring-shaped
rashes.
- Erythema chronicum
migrans (ECM)
- Expanding red ring
with clearer centre.
- Fever, chills, muscle
pains and headaches.
- ECM is due to a spiral
shaped bacteria called Borrelia burgdorferi which is transmitted
by tick bites. It is more common in the US and Parts of Europe.
-
- Erythema annulare
centrifugum
- Expanding red ring-shaped
patch with a scaly border lagging behind. Lasts weeks to years.
- May be associated
with fungal infection, parasitic bowel disease or autoimmune
disorders.
-
- Erythema gyratum
repens
- Red ring-shaped rashes
that are arranged in a wood-grain pattern.
- Usually associated
with underlying cancer.
-
- Erythema marginatum
- Red ring-shaped rashes
that change in size and shape.
- A sign of rheumatic
fever, a streptococcal bacterial infection that causes arthritis,
heart valve inflammation and fever.
What you can do
- You should consult
a doctor.
What the doctor
may do
- Perform investigations
to determine the cause, if any.
- Treat the cause.
TOP
APHTHOUS
ULCERS
Aphthous ulcers or
canker sores are common mouth ulcers that affect at least 20%
of the population. They occur most frequently during early adult
life and become less common with age. The ulcers number from
1 - 5 and heal spontaneously after 1 - 2 weeks but often recur.
TOP
APLASIA
CUTIS
Aplasia cutis refers
to the congenital absence of skin. It occurs in newborns and
is sometimes blamed on forceps, if used to assist delivery.
Cause
- Developmental abnormality
in which skin fails to develop over localised areas such as the
scalp.
Symptoms
- Appears at birth.
- Usually occurs on
the scalp and rarely on other parts of the body.
- It appears as an ulcer
which is raw or covered by a crust or as a depressed area covered
by a tough smooth membrane.
- The raw area eventually
heals leaving a flat or raised scar.
- Hairs are absent over
the affected area.
- Aplasia cutis may
sometimes be associated with trisomy 13, a chromosomal disorder.
Complications
- Secondary bacterial
infection.
- Haemorrhage.
What you can do
- You should consult
a doctor.
What the doctor
may do
- Confirm the diagnosis.
- Treat the complications.
- Surgically remove
the affected area if healing is poor or for cosmetic reasons.
TOP
ATOPIC DERMATITIS
Atopic dermatitis is
a type of eczema that occurs in people with a family history
of allergic conditions such as asthma (wheezy breathing), allergic
rhinitis (itchy, runny nose) and atopic dermatitis. Atopic is
the adjective for "atopy" which is an inherited predisposition
to hypersensitivity reactions in the skin (atopic dermatitis),
bronchi or breathing tubes (asthma) and allergic rhinitis (nasal
passages). Atopic dermatitis usually occurs between the 2 months
and 2 years of age and improves with age so that 80 - 90% of
those affected are very much improved by the time they reach
puberty. The sites most commonly affected include the face, neck,
front of the elbows and behind the knees. Atopic dermatitis is
estimated to affect 3% of children.
Cause
- The atopic tendency
or predisposition to asthma, allergic rhinitis and atopic dermatitis
is believed to be inherited. However, this tendency is not specific
which means that a parent with atopic dermatitis may have an
offspring with asthma rather than atopic dermatitis or vice versa.
Two-thirds of patients give a personal or family history of asthma,
allergic rhinitis or atopic dermatitis.
Symptoms
- In young children,
atopic dermatitis usually affects the face, scalp, napkin areas
and limbs or it can be quite generalised
- In older children
and adults, it usually affects the neck and front of the elbows
and back of the knees.
- Itch is usually severe
and there are often scratch marks and even bleeding points. Scratching
make the dermatitis worse so an itch-scratch-rash cycle develops,
causing the dermatitis to flare suddenly. Constant scratching
leads to lichenification (leathery thickened and darkened skin).
- Recurrences are characteristic.
The other signs are:
-
- Acute eczema - redness, papules (pimply
bumps), weeping, crusting and broken skin due to scratching.
- Chronic eczema - dry, scaly and lichenified
(leathery thickened and often darkened) skin.
 |
Atopic dermatitis affecting
the front of the elbows.
Click
on image for larger view. |
 |
Atopic dermatitis
affecting the backs of the knees.
Click
on image for larger view. |
Complications
- Bacterial infection
due to scratching.
- Herpes simplex virus
infection ("cold sores") leading to eczema
herpeticum.
- Increased susceptibility
to warts and molluscum
contagiosum.
What you can do
- You should consult
a doctor for treatment and advice.
- Take simple antihistamines
to relief itch.
- Avoid over-drying
the skin (see preventing dryness below).
- Avoid rough textured
fabrics.
- Avoid foods that appear
to aggravate the eczema.
- Cut the fingernails
short so as to reduce trauma to the skin. Mittens can be worn
at night for the same purpose.
- Take Evening Primrose
Oil or Borage Oil (types of health food) which may sometimes
help to reduce the severity of atopic dermatitis.
- Stress is a common
cause of relapse. Confront and deal with stresses.
- Keep away from persons
with active herpes
simplex virus infection ("cold sores").
- Avoid careers which
involve excessive exposure to heat, chemicals and degreasing
agents; for example, hairdressing, nursing or industrial work.
- Avoid hot humid jobs.
Preventing dryness
- Avoid long, hot baths.
Instead take short warm showers.
- Avoid soap or use
emulsifying ointment in place of soap.
- If you find not using
soaps unpalatable, use a mild dermatological soap or bath oil
instead.
- Apply moisturisers
after baths/showers and as frequently as necessary.
What the doctor
may do
- Prescribe topical
steroids and in severe cases, even oral steroids and cyclosporin
(an immunosuppressive
drugs used to prevent the rejection of transplanted organs).
PUVA may be used in adults
with very resistant atopic dermatitis.
- Hospitalise severe
cases for treatment and rest. Severe eczema can sometimes improve
in response to a change in the environment alone.
- Prescribe antibiotics
for secondary bacterial infection.
- Perform skin
tests (prick or intradermal tests) and RAST
to exclude food allergies in selected cases.
- Advise elimination
diets in selected cases. A small proportion (about 10%) of children
with atopic dermatitis have food allergies and improve when the
offending food is eliminated from the diet. Some of the foods
reported to cause allergies include eggs, cow's milk, nuts and
fish. Because many of these foods have superior nutritional value,
elimination diets are generally used only under a doctor's supervision
and when simple treatments do not work.
TOP
ATROPHIE BLANCHE
Atrophie means thinned and blanche
means white. The term atrophie blanche therefore, means thinned
white scars.
Cause
- Healed leg ulcers
from vasculitis or stasis ulcers.
- Livedo vasculitis.
Symptoms
- Thinned white scars
with red spots or telangiectasias
(broken capillaries).
What you can do
- You should consult
a doctor.
What the doctor
may do
- Treat with drugs that
prevent the aggregation of platelets such as aspirin, pyridamole
and pentoxyfylline.
TOP |